Lumbar Disk Disease (Herniated Disk)
What is lumbar disk disease?
The vertebral column, also called the backbone, is made up of 33 vertebrae that are separated by spongy discs. The spine is divided into 4 distinct areas from top to bottom:
- Cervical spine: The first 7 vertebrae, located in the neck
- Thoracic spine: The next 12 vertebrae, located in the chest area
- Lumbar spine: The next 5 vertebrae, located in the lower back
- Sacral spine: The lowest 5 vertebrae, located below the waist
The lumbar spine consists of 5 bony segments in the lower back area, which is where lumbar disk disease occurs.
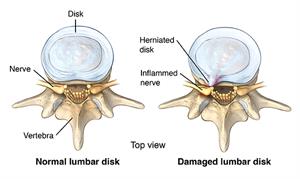
- Bulging disk. With age, the intervertebral disk may lose fluid and become dried out. As this happens, the spongy disk (which is located between the bony parts of the spine and acts as a “shock absorber”) becomes compressed. This may lead to the deterioration of the tough outer ring allowing the nucleus, or the inside of the ring, to bulge out. This is called a bulging disk.
- Ruptured or herniated disk. As the disk continues to break down, or with continued stress on the spine, the inner nucleus pulposus may actually rupture out from the annulus. This is a ruptured, or herniated, disk. The fragments of disc material can then press on the nerve roots located just behind the disk space. This can cause pain, weakness, numbness, or changes in sensation.
Most disk herniations happen in the lower lumbar spine, especially between the fourth and fifth lumbar vertebrae and between the fifth lumbar vertebra and the first sacral vertebra (the L4-5 and L5-S1 levels).
What causes lumbar disk disease?
Lumbar disk disease is caused by a change in the structure of the normal disk. Most of the time, disk disease happens as a result of aging and the normal degeneration that occurs within the disk. Occasionally, severe injury can cause a normal disk to herniate. Injury may also cause an already herniated disk to worsen.
What are the risks for lumbar disk disease?
Although age is the most common risk, physical inactivity can cause weak back and abdominal muscles, which may not support the spine properly. Back injuries also increase when people who are normally physical inactive participate in overly strenuous activities. Jobs that require heavy lifting and twisting of the spine can also cause back injuries.
What are the symptoms of lumbar disk disease?
The symptoms of lumbar disk disease vary depending on where the disk has herniated, and what nerve root it is pushing on. The following are the most common symptoms of lumbar disk disease. However, each person may experience different symptoms. Symptoms may include:
- Intermittent or continuous back pain. This may be made worse by movement, coughing, sneezing, or standing for long periods of time
- Spasm of the back muscles
- Sciatica – pain that starts near the back or buttock and travels down the leg to the calf or into the foot
- Muscle weakness in the legs
- Numbness in the leg or foot
- Decreased reflexes at the knee or ankle
- Changes in bladder or bowel function
The symptoms of lumbar disc disease may resemble other conditions or medical problems. Always see your health care provider for a diagnosis.
How is lumbar disk disease diagnosed?
In addition to a complete medical history and physical exam, you may have one or more of the following tests:
- X-ray. A diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film.
- Magnetic resonance imaging (MRI). A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body.
- Myelogram. A procedure that uses dye injected into the spinal canal to make the structure clearly visible on X-rays.
- Computed tomography scan (also called a CT or CAT scan). A diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
- Electromyography (EMG). A diagnostic test that measures muscle response or electrical activity in response to a nerve’s stimulation of the muscle.
How is lumbar disk disease treated?
Specific treatment for lumbar disk disease will be determined by your health care provider based on:
- Your age, overall health, and medical history
- Extent of the condition
- Type of condition
- Your tolerance for specific medications, procedures, or therapies
- Expectations for the course of the condition
- Your opinion or preference
Typically, conservative therapy is the first line of treatment to manage lumbar disk disease. This may include a combination of the following:
- Bed rest
- Education on proper body mechanics (to help decrease the chance of worsening pain or damage to the disk)
- Physical therapy, which may include ultrasound, massage, conditioning, and exercise programs
- Weight control
- Use of a lumbosacral back support
- Medications (to control pain and/or to relax muscles)
If these conservative measures fail, you may need surgery to remove the herniated disc. Surgery is done under general anesthesia. Your surgeon will make an incision in your lower back over the area where the disc is herniated. Some bone from the back of the spine may be removed to gain access to the area where the disc is located. Your surgeon will remove the herniated part of the disc and any extra loose pieces from the disc space.
After surgery, you may be restricted from activity for several weeks while you heal to prevent another disc herniation. Your surgeon will discuss any restrictions with you.
What are the complications of lumbar disk disease?
Lumbar disk disease can cause back and leg pain that interferes with daily activities. It can lead to leg weakness or numbness and difficulty with bowel and bladder control.
Can lumbar disk disease be prevented?
Maintaining a healthy weight, participating in regular exercises, and using good posture can minimize your risk for lumbar disk disease.
Living with lumbar disk disease
Conservative therapy requires patience; but sticking with your treatment plan can reduce back pain and minimize the chance of worsening pain or damage to the disk. Conservative measures and surgery can both take time to be effective.
When should I call my health care provider?
Notify your health care provider if your pain increases or if you begin having difficulty with bowel or bladder control.
Key points
- Lumbar disk disease may occur when a disc in the lumbar area of the spine bulges or herniates from between the bony area of the spine.
- Lumbar disk disease causes lower back pain and leg pain and weakness that is made worse by movement and activity.
- The first step in treatment to reduce pain and reduce increasing pain or injury to the spine.
- Surgery may be considered if the more conservative therapy fails.
Next steps
Tips to help you get the most from a visit to your health care provider:
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the names of new medicines, treatments, or tests, and any new instructions your provider gives you.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Online Medical Reviewer: Foster, Sara, RN, MPH
Online Medical Reviewer: Freeborn, Donna, PhD, CNM, FNP
Date Last Reviewed: 1/14/2014
© 2000-2016 The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.